This post is taken from my other blog, Golf Rehab Doc. Check it out if you are interested in rehab, injuries, and performance information specific to golf. To go to the site click —> HERE. Thanks for reading!
Low back pain (LBP) is consistently cited as the most common injury among golfers. This statistic has lead many researchers to conduct studies and formulate correlations between LBP, physical characteristics of the golfer and swing faults. However, it should be noted that many authors admit that LBP is a multifaceted condition that is difficult to control in scientific research. Furthermore, it is not within the scope of this post to review the anatomy and pathophysiology behind different medical diagnoses (ex. disc herniation, muscle strain, etc.) in regard to low back pain. However, it has been well documented that treatment should not performed with only the medical diagnosis in mind and that each individual should be evaluated. With that said, the following is a summary of different mechanisms that have been found to contribute to low back pain in golfers.
RANGE OF MOTION
- Hip Internal Rotation: It has been concluded that decreased lead hip IR may contribute to LBP in golfers.
- This was found in both pros and amateurs.
- Reduced hip IR may cause compensation of over rotation of the trunk.
- Likewise, improving lead hip IR has been found to reduce low back pain (Grimshaw and Burden, 2000)
- To start the process of testing your hip internal rotation click —> HERE
- Hip External Rotation: There is an established correlation between decreased lead hip FABER range of motion and LBP.
- This was only for professional golfers, but not for amateurs.
- Non-Lead Hip Range of Motion: No correlation in amateurs or professional golfers.
- Lumbar Extension: Decreased lumbar extension has been shown to correlate to a history of LBP.
- The test for this is an easy one. Lay on your stomach (prone) and place your hands under your shoulders as if you were going to do a push-up. Without lifting your pelvis off of the table, straighten your arms as if to stretch your back. If you are unable to full extend your elbow (or come close to it) without having your pelvis rise off of the ground, you have limited lumbar extension.
- Lumbar Flexion: There was no correlation between decreased lumbar flexion ROM and a history of LBP.
- Trunk (Thoracic) Rotation: Golfers with LBP have less rotational flexibility in the trunk (Lindsay and Horton, 2002).
- How can I test my trunk rotation? Glad you asked. Click —> HERE.
- The test video from TPI does not fully isolate the thoracic spine, but it can tell us if we need to assess further to isolate the thoracic spine.
- Toe Touch: An inability to perform a toe touch was also related to LBP in one article. To see how to perform this test click —> HERE.
SWING FAULTS
- Reverse Spine Angle: Usually a compensatory pattern that results from decreased hip or trunk rotation (see above).
- For an example of this swing fault, check out this video from TPI —> HERE.
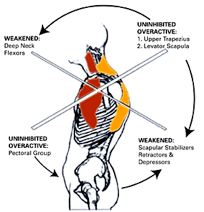
- S – Posture: In the world of orthopedics, this is also called lumbar lordosis. It has also been coined “lower-crossed syndrome.”
- This posture places the lumbar spine in hyper-extension and a video example is —> HERE.
- C – Posture: This is a posture that places the lumbar spine in flexion.
- Hanging Back: Considered to be a potential swing fault for various reasons, I find it is due to lack of lead hip internal rotation or lack of stability/ balance on the left leg.
- This lack of hip internal rotation or stability decreases the player’s ability to transition to the lead side and complete the follow-through.
- A great demonstration is found —> HERE.
- Early Extension: Another swing fault due to reduced lead hip internal rotation. There are physical parameters and screens that correlate to this swing fault. However, here is an in depth overview of this swing fault —> HERE.
MUSCLE STRENGTH/ STABILITY
Even though range of motion and technique is very important in the golf swing to protect the spine, we cannot forget about strength and stability in the lower extremity and core. It is well documented that strength and power can improve performance, but we need to remember that it can also reduce the risk of injury. Without going into excessive detail, the lower body and core should have adequate stability in order to attenuate considerable amounts of load on the spine during the back-swing, impact, and follow through. Several tests can be helpful to detect core and lower extremity stability deficits.
- Single Leg Stance: a test for overall balance that can highlight any side to side asymmetries —> Click HERE.
- Bride with Leg Extension Test: a great test for lumbo-pelvic-core stability especially gluteal function is shown —> HERE.
- Trunk Stability Push-Up: tests the ability to stabilize the spine in an anterior and posterior plane during a closed-chain upper body movement. An overview of this test is —> HERE and reasons why its important are —> HERE.
Resources
Grimshaw, P., Burden, A. M. (2000). Case Report: reduction of low back pain in a professional golfer. Medicine & Science in Sports & Exercise, 32, 1667-1673.
Lindsey, D., Horton, J. (2002). Comparison of spine motion in elite golfers with and without low back pain. Journal of Sports Science, 20, 599-605.
Murray E, Birley E, Twycross-Lewis R, Morrissey D. The relationship between hip rotation range of movement and low back pain prevalence in amateur golfers: an observational study. Phys Ther Sport. 2009;10(4):131-135.
Vad, V. B. (2004). Low back pain in professional golfers: the role of associated hip and low back range-of-motion deficits. American Journal of Sports Medicine, 32, 494-497.